- Using the ALS treatment algorithm
Step 2
Learning outcomes
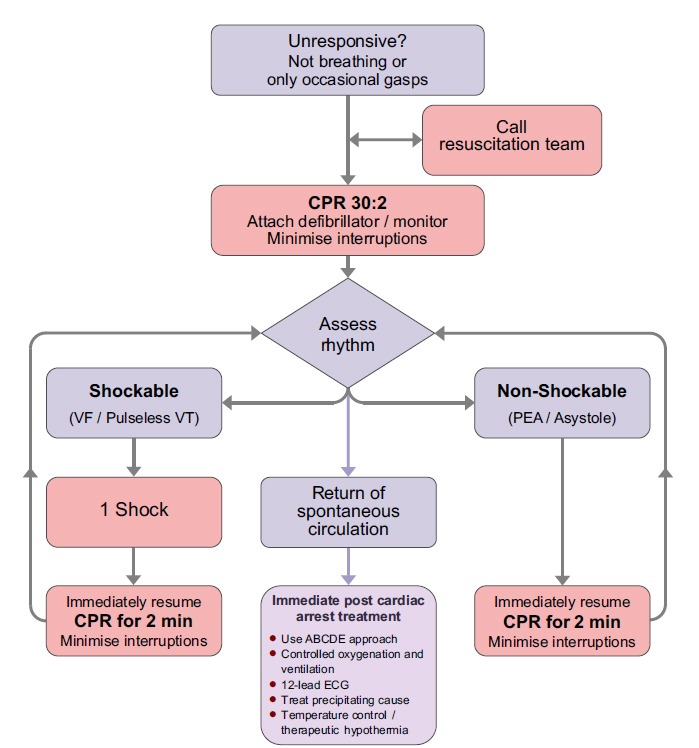
- The ALS algorithm
- Importance of high quality chest compressions
- Treatment of shockable and non-shockable rhythms
- Administration of drugs during cardiac arrest
- Potentially reversible causes of cardiac arrest
- Role of resuscitation team
Return to top
Step 4
To confirm cardiac arrest...
- Patient response
- Open airway
- Check for normal breathing
- caution agonal breathing
- Check circulation
- Monitoring
Return to top
Step 7

Chest compression
- 30:2
- Compressions
- centre of chest
- 5-6 cm depth
- 2 per second (100-120 min-1)
- Maintain high quality compressions with minimal interruptions
- Continuous compressions once airway secured
- Switch CPR provider every 2 min cycle to avoid fatigue
Return to top
Step 9
- Bizarre irregular waveform
- No recognisable QRS complexes
- Random frequency and amplitude
- Uncoordinated electrical activity
- Coarse/fine
- Exclude artefact
- movement
- electrical interference
Return to top
Step 11
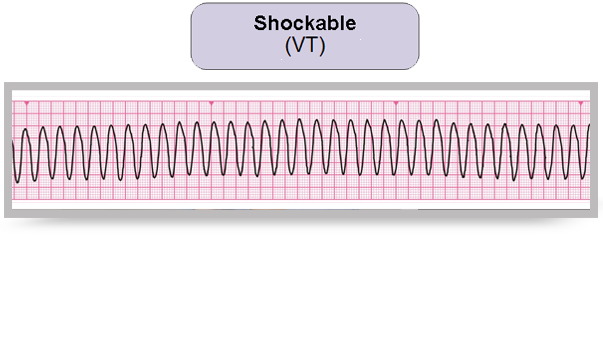
- Monomorphic VT
- broad complex rhythm
- rapid rate
- constant QRS morphology
- Polymorphic VT
- torsade de pointes
Return to top
Step 17
Defibrillation energies
- Vary with manufacturer
- Check local equipment
- If unsure, deliver highest available energy
- DO NOT DELAY SHOCK
- Energy levels for defibrillators will be given on your course
Return to top
Step 18
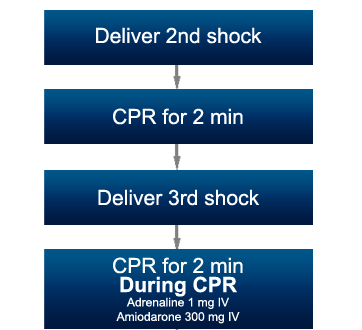
If VF / VT persists
- 2nd and subsequent shocks
- 150 – 360 J biphasic
- 360 J monophasic
- Give adrenaline and amiodarone after 3rd shock during CPR
Return to top
Step 20
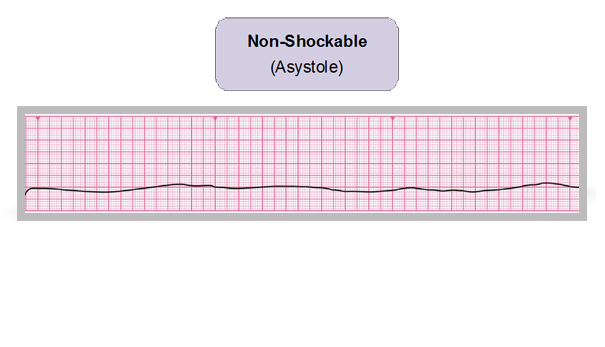
- Absent ventricular (QRS) activity
- Atrial activity (P waves) may persist
- Rarely a straight line trace
- Adrenaline 1 mg IV then every 3-5 min
Return to top
Step 21
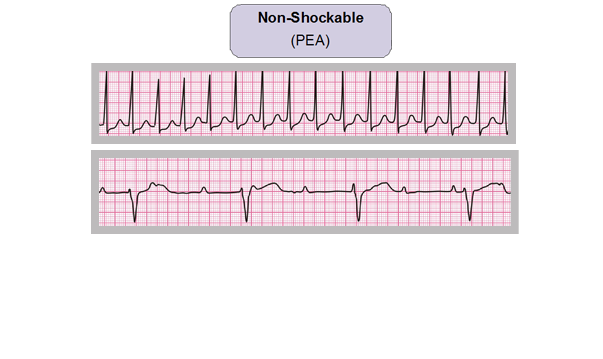
- Clinical features of cardiac arrest
- ECG normally associated with an output
- Adrenaline 1 mg IV then every 3-5 min
Return to top
Step 23
During CPR
- Ensure high-quality CPR: rate, depth, recoil
- Plan actions before interrupting CPR
- Give oxygen
- Consider advanced airway and capnography
- Continuous chest compressions when advanced airway in place
- Vascular access (intravenous, intraosseous)
- Give adrenaline every 3-5 min
- Correct reversible causes
Return to top
Step 24
Airway and ventilation
- Secure airway:
- supraglottic airway device e.g. LMA, i-gel
- tracheal tube
- Do not attempt intubation unless trained and competent to do so
- Once airway secured, if possible, do not interrupt chest compressions for ventilation
- Avoid hyperventilation
- Capnography
Return to top
Step 27

Hypoxia
- Ensure patent airway
- Give high-flow supplemental oxygen
- Avoid hyperventilation
Return to top
Step 28

Hypovolaemia
- Seek evidence of hypovolaemia
- history
- examination
- internal haemorrhage
- external haemorrhage
- check surgical drains
- Control haemorrhage
- If hypovolaemia suspected give intravenous fluids
Return to top
Step 29
Hypo/hyperkalaemia and
metabolic disorders
- Near patient testing for K+ and glucose
- Check latest laboratory results
- Hyperkalaemia
- calcium chloride
- insulin/dextrose
- Hypokalaemia/hypomagnesaemia
- electrolyte supplementation
Return to top
Step 30

Hypothermia
- Rare if patient is an in-patient
- Use low reading thermometer
- Treat with active re-warming techniques
- Consider cardiopulmonary bypass
Return to top
Step 31
Tension pneumothorax
- Check tube position if intubated
- Clinical signs
- decreased breath sounds
- hyper-resonant percussion note
- tracheal deviation
- Initial treatment with needle decompression or thoracostomy
Return to top
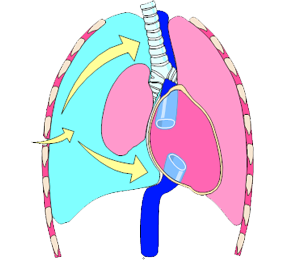
Step 32
Tamponade, cardiac
- Difficult to diagnose without echocardiography
- Consider if penetrating chest trauma or after cardiac surgery
- Treat with needle pericardiocentesis or resuscitative thoracotomy
Return to top
Step 34
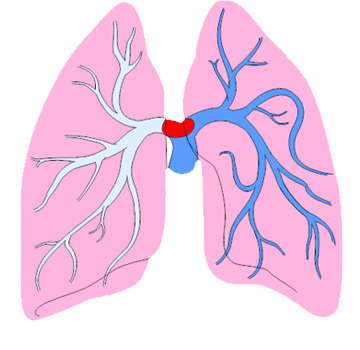
Thrombosis
- If high clinical probability for PE consider fibrinolytic therapy
- If fibrinolytic therapy given continue CPR for up to 60-90 min before discontinuing resuscitation
Return to top
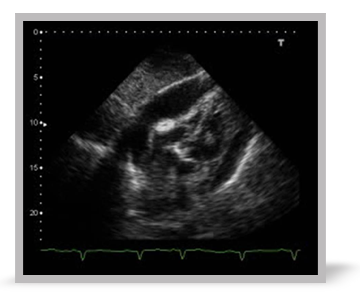
Step 35

Ultrasound
- In skilled hands may identify reversible causes
- Obtain images during rhythm checks
- Do not interrupt CPR
Return to top
Step 37

Resuscitation team
- Roles planned in advance
- Identify team leader
- Importance of non-technical skills
- task management
- team working
- situational awareness
- decision making
- Structured communication
Return to top
Step 38
Summary
- The ALS algorithm
- Importance of high quality chest compressions
- Treatment of shockable and non-shockable rhythms
- Administration of drugs during cardiac arrest
- Potentially reversible causes of cardiac arrest
- Role of resuscitation team
Return to top
Step 39
Advanced Life Support Course
E-lecture
All rights reserved
© Resuscitation Council (UK) 2011
Return to top
Transcript
1. Welcome to the ALS algorithm lecture.
2. The aim of this lecture is to:
- Outline the ALS treatment algorithm
- Emphasise the importance of high quality chest compressions
- Outline the treatment algorithms for shockable and non-shockable rhythms
- Describe the role of drugs during cardiac arrest
- Outline the potentially reversible causes of cardiac arrest
- Consider the role of the resuscitation team.
3. The ALS treatment algorithm provides a standardised approach to the resuscitation of the adult patient in cardiac arrest. It is a central element in the ALS course.
The strengths of this protocolised approach are its foundations from the 2010 International Liaison Committee for Resuscitation scientific evidence evaluation process and the fact that it provides a common standard from which resuscitation providers can make rapid treatment decisions in an emergency situation. It provides focus on the task in hand and allows all members of the team to work from the same standard, allowing them to anticipate and plan for interventions.
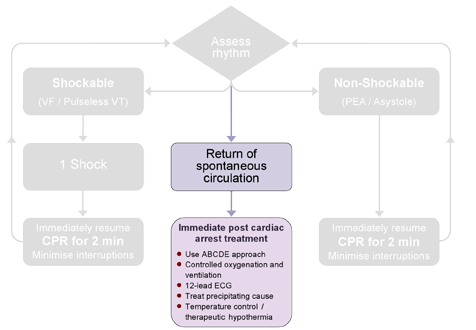
This slide show the ALS treatment algorithm in its entirety. It takes the ALS provider through the initial assessment of the unresponsive patient, commencement of CPR and management according to the initial rhythm, before outlining the key stages after achieving return of spontaneous circulation.
Over the course of the next few slides I am going to break this down into stages.
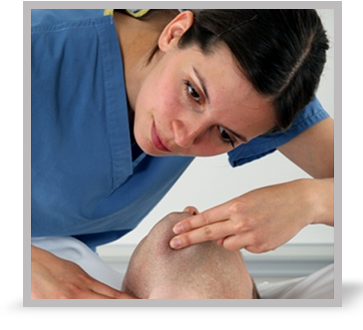
4. The first step in the assessment process is to test for the patient’s response. If they are unresponsive, open their airway and check for normal breathing. Take care not to confuse normal breathing with agonal breathing. This is slow, sighing respirations and is common in the early stages after cardiac arrest. It should not be confused with signs of life. Simultaneously with breathing assessment, check for other signs of life, e.g. coughing or movement - this should include checking for the carotid pulse. Use any monitoring attached to the patient to assist in the decision making process.
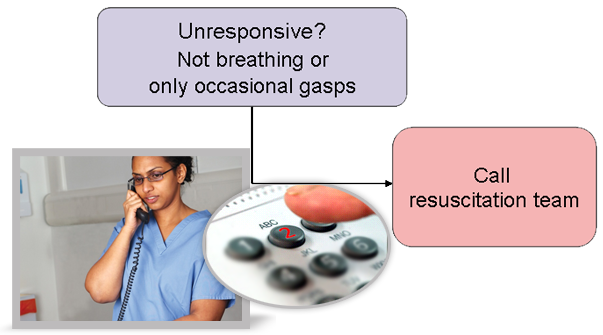
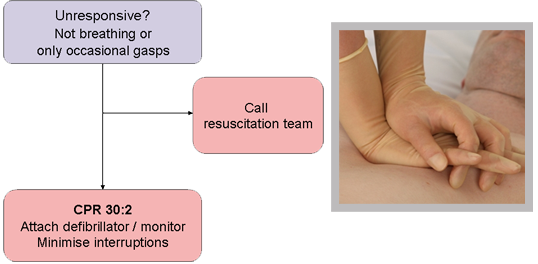
5. The diagnosis of cardiac arrest is based on the patient being unresponsive and either not breathing or only having occasional gasps.
Once cardiac arrest is confirmed, alert other staff in the area. This can be done by activating the emergency alarm or calling for help. Send a member of staff to call the resuscitation team unless they are already in attendance. Be explicit in your briefing to the person you send to make the emergency call ensuring the person knows the location, nature of emergency and response required. Imprecise instructions such as, “Put the call out” or “Call the crash team” can lead to confusion.
In the UK, hospitals use a centralised emergency call number which is 2222. Give clear concise instructions to the telephone operator ensuring that the location, nature of emergency and response required are clearly stated. For example a good call would state, “There is a cardiac arrest on ward 4. Please send the cardiac arrest team”. It is good practice for the switchboard operator to confirm the details before placing the emergency call.
6. While the resuscitation team are being called, ensure CPR is commenced without delay. Start with 30 chest compressions followed by 2 ventilations. Attach the defibrillator/monitor as soon as it is available.
7. There is good evidence that the quality of chest compressions and ventilations is related to patient outcome.
Alternate 30 high quality chest compressions with 2 ventilations.
Ensure compressions are given in the centre of the chest, to a depth of 5-6 cm at a rate of approximately 100-120 min-1. Allow the chest to fully re-expand between compressions and avoid residual pressure on the chest between compressions.
Even brief interruptions in chest compressions are harmful and should be avoided.
Once the airway is secured switch to continuous chest compressions with asynchronous ventilation.
The quality of CPR declines as CPR providers become fatigued. To avoid fatigue switch the CPR provider every 2 minutes.
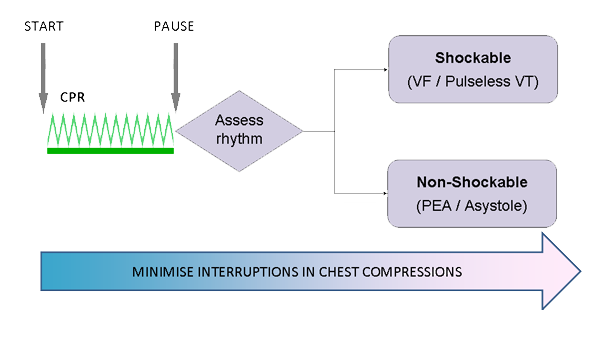
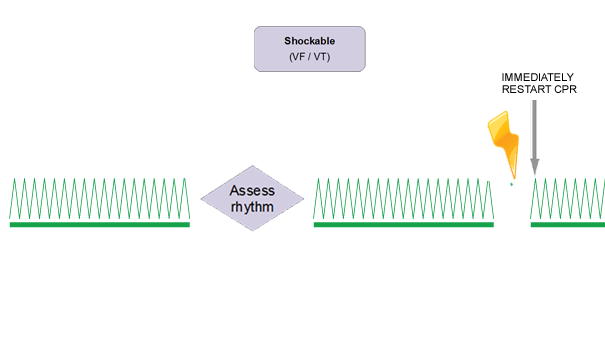
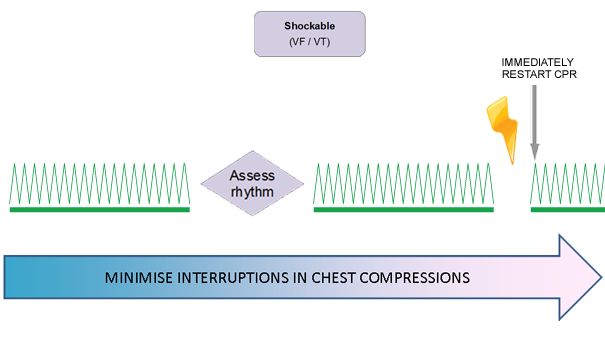
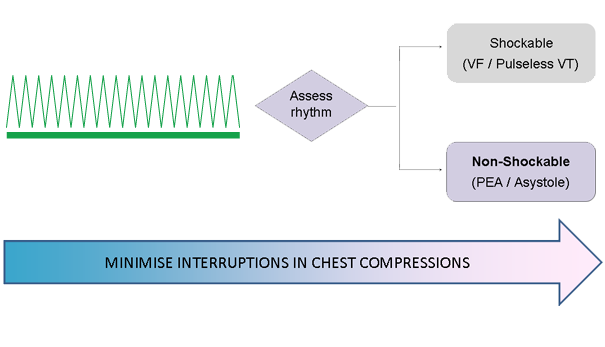
8. Once the defibrillator is attached, briefly pause to assess the underlying rhythm. Keep the time spent analysing the rhythm as short as possible and certainly avoid interruptions in CPR of greater than 10 seconds duration. Once you have determined if a shockable or non-shockable rhythm is present, re-start CPR.
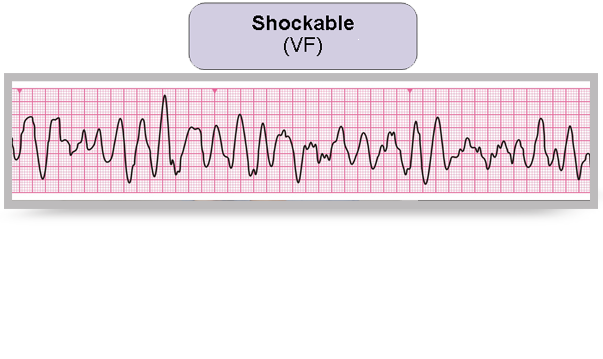
9. Ventricular fibrillation is a shockable rhythm. It is characterised by bizarre irregular waveform with no recognisable QRS complexes. There is no pattern to the frequency or amplitude giving the appearance of uncoordinated electrical activity.
The amplitude (or size) of the ECG trace can lead to VF being described as either coarse or fine. Very fine VF rarely responds to a shock and will eventually degenerate into asystole. If you are uncertain whether there is fine VF or asystole, treat as asystole and continue CPR.
Be aware that movement or electrical interference can on occasion give rise to an ECG that could look like VF.
10. Ventricular tachycardia is the other shockable rhythm.
Monomorphic VT is a characterised by broad QRS complexes, rapid rate and constant QRS morphology.
11. Polymorphic VT is characterised by a cyclical increasing and decreasing waveform amplitude.
If the patient is in cardiac arrest, treat both rhythms as if they are VF.
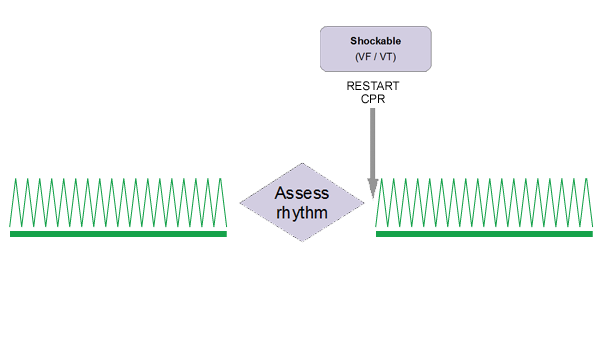
12. Once a shockable rhythm is identified, restart CPR and prepare the team to deliver a shock. It is important to minimise the hands off time both before and after delivering a shock as prolonged pre and post-shock pauses reduces shock efficacy.
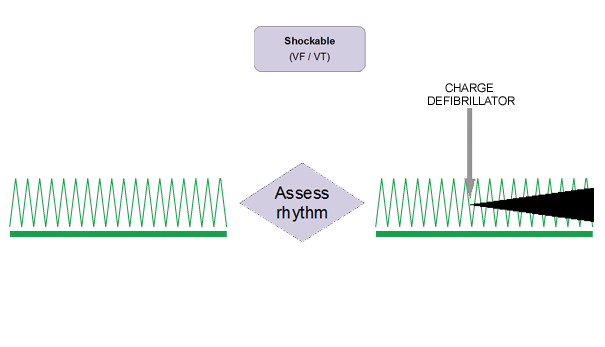
13. To facilitate keeping pre-shock pauses to a minimum, charge the defibrillator during CPR. Ensure all other team members are clear of the patient during charging.
This sequence requires careful co-ordination of the resuscitation team and clear communication between the team leader, CPR provider and defibrillator operator.
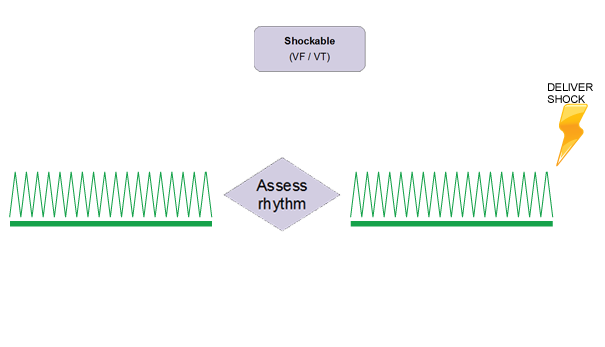
14. When the defibrillator is charged, the team and CPR provider stand clear of the chest and the shock is delivered without pausing to recheck the rhythm.
15. As soon as the shock is delivered, restart CPR immediately and continue for a further 2 minutes.
16. Throughout the shock sequence minimise interruptions in chest compressions.
17. Defibrillation energies vary between different types of defibrillators. Ensure you are familiar with the equipment in your own institution.
If you are unsure, give the highest available energy and do not delay the shock trying to decide on the correct energy level.
When you attend your face to face part of the course you will be told about the appropriate energy levels for the specific type of defibrillators being used on your course.
18. If after 2 minutes of high quality CPR, VF/VT persists give a second shock and restart CPR for a further 2 minutes. If VF/VT still persists then give a third shock and restart CPR. After the third shock give adrenaline 1 mg IV and amiodarone 300 mg IV.
It is important in shock-refractory VF/VT to check the position and contact of the defibrillation pads. The duration of any individual resuscitation attempt is a matter of clinical judgement, and should take into account the perceived prospect of a successful outcome. If it was considered appropriate to start resuscitation, it is usually considered worthwhile continuing as long as the patient remains in identifiable VF/VT. Seek expert help in this situation.
19. I am going to move now from considering the shockable to the non-shockable rhythms.
There are two non-shockable rhythms – PEA and asystole.
20. Asystole is characterised by absent ventricular activity. Occasionally atrial activity may persist. Unlike true asystole, isolated P wave activity may respond to pacing.
If a completely straight line is seen check the defibrillator setting is correct and leads/pads are appropriately attached.
Asystole is treated by providing good quality CPR, identification and treatment of reverisble causes and administering 1mg IV adrenaline. Repeat doses may be given every 3-5 minutes.
21. Pulseless electrical activity (PEA) is defined as organised cardiac electrical activity in the absence of any palpable pulses. These patients often have some mechanical myocardial contractions but they are too weak to produce a detectable pulse or blood pressure.
PEA may be caused by reversible conditions that can be treated. Survival following cardiac arrest with asystole or PEA is unlikely unless a reversible cause can be found and treated quickly and effectively.
Treatment of PEA focuses on high quality CPR, identification and treatment of reversible causes and adrenaline every 3-5 minutes.
22. During CPR ensure attention is paid to maintaining high quality chest compressions.
Pause for a moment and write down the characteristics of high quality chest compressions.
23. The key characteristics are compression rate 100-120 min-1; depth 5-6 cm; allowing full chest recoil between compressions and minimising interruptions.
Give high concentration oxygen and consider an advanced airway.
24. We will now take a moment to focus on these other interventions.
The airway may be secured with a supraglottic device such as an LMA or i-gel or a tracheal tube. Whilst attempting to secure the airway avoid anything but brief interruptions in chest compressions.
There is no definitive evidence demonstrating a survival benefit for tracheal intubation over and above other airway interventions. Tracheal intubation in a patient in cardiac arrest is technically challenging. An un-recognised oesophageal intubation will be fatal. Do not attempt intubation unless trained and competent to do so.
Once airway secured, it may be possible to perform continuous compressions without pausing for ventilation. This will reduce interruptions in chest compressions. Ventilate the lungs at 10 breaths min-1 and avoid hyperventilation.
If excessive gas leakage causes inadequate ventilation of the patient’s lungs, chest compressions will have to be interrupted to enable ventilation (using a chest compression:ventilation ratio of 30:2). Capnography may be used to confirm tube placement and monitor the quality of CPR. A rapid rise in ETCO2 may be an early sign of ROSC.
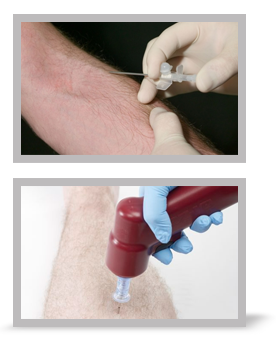
25. Although the time taken for drugs to reach the central circulation is longer for peripheral rather than centrally administered drugs, the risk of complications from inserting a central line during CPR is high.
Unless the patient has a pre-existing, patent central line, peripheral venous access is the route of choice for administering drugs in cardiac arrest. Follow all injections of drugs with at least a 20ml bolus of fluid and elevate the limb if possible.
If intravenous access cannot be established within the first two minutes of resuscitation, consider gaining intraosseous (IO) access.
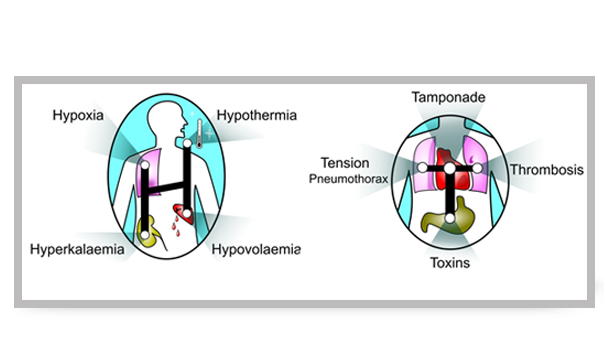
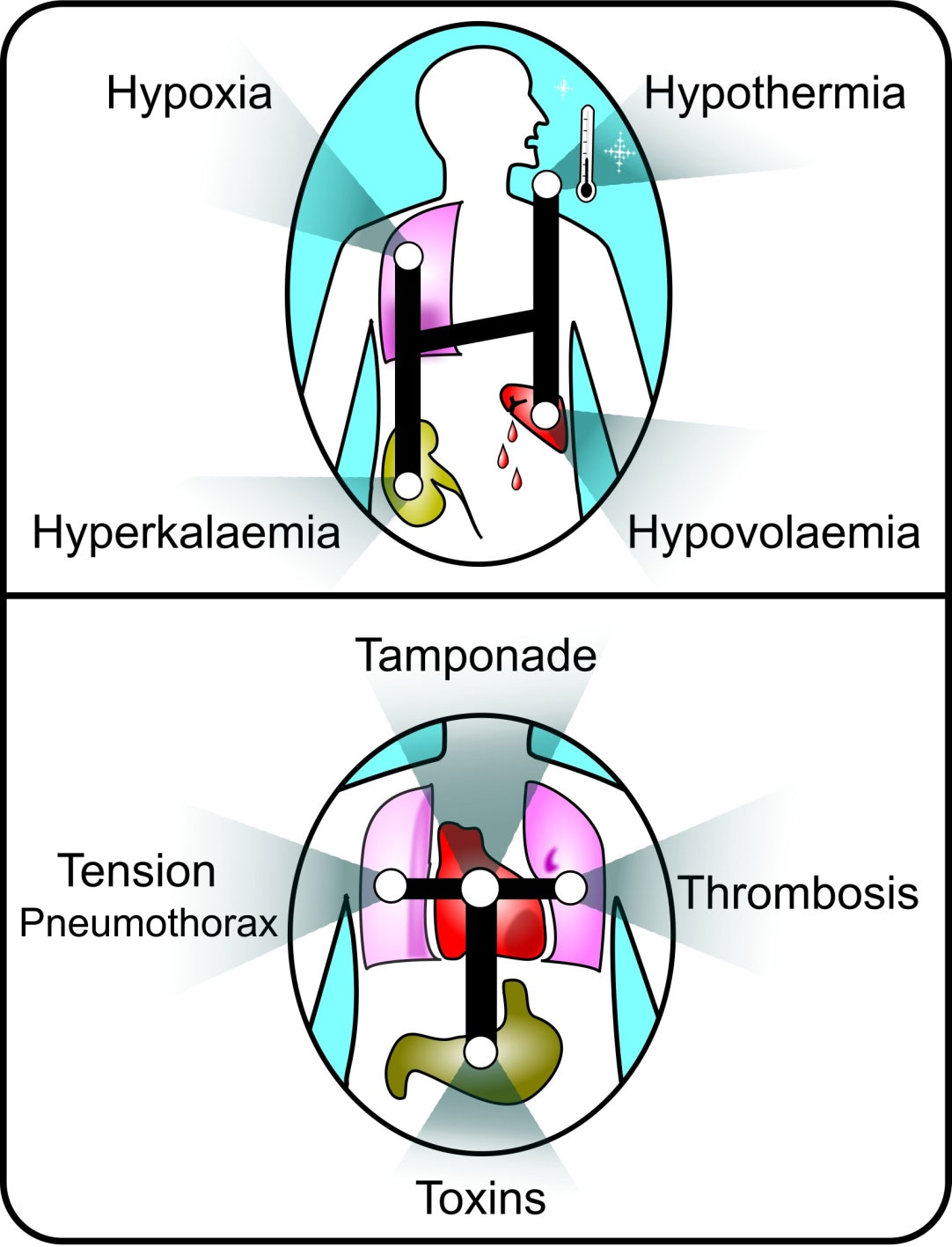
26. Potential causes of cardiac arrest for which specific treatment exists must always be considered. For ease of memory, these are divided into two groups of four based upon their initial letter — either H or T. These are often referred to as the 4 Hs and the 4 Ts. It is important to consider and address the relevant causes first.
27. Treat hypoxia by ensuring the airway is patent. Ventilate the lungs using high flow supplemental oxygen.
Although it has been common practice to hyperventilate a patient in cardiac arrest based on the premise that this will blow off excess CO2, this practice should be avoided as hyperventilation reduces coronary perfusion pressure and worsens outcome.
28. Clues to hypovolaemia may come from the patient history, review of observation charts or clinical examination. Evidence of hypovolaemia may be obvious such as internal or external haemorrhage, blood in drains or more subtle, such as severe sepsis or anaphylaxis.
If hypovolaemia is suspected, rapidly infuse intravenous fluids.
29. The next H covers electrolyte and metabolic disorders.
Near patient testing equipment allows the rapid measurement of potassium and glucose.
Review the patient’s latest laboratory results.
Immediate treatment of hyperkalaemia is administration of calcium chloride followed by insulin/dextrose infusion.
Low potassium/magnesium levels may be treated with electrolyte infusions.
30. Hypothermia is rare as a cause of cardiac arrest if the patient is an in-patient.
Measure core temperature with a low reading thermometer.
Treatment of the hypothermic patient in cardiac arrest will require active re-warming techniques.
Cardiopulmonary bypass may be considered if facilities are immediately available or if active re-warming strategies fail.
31. Next we move on to the Ts, starting with tension pneumothorax.
In the intubated patient check tube position as intubation of the right main bronchus can complicate the diagnosis of tension pneumothorax.
Clinical signs of a tension pneumothorax comprise decreased breath sounds and hyper-resonant percussion note on the side of the pneumothorax. The mediastinum will be shifted to the contralateral side which gives rise to the clinical sign of tracheal deviation away from the side of the pneumothorax.
Treat with needle decompression. Be aware that chest wall thickness may exceed standard cannula lengths. If this is suspected perform a thoracostomy.
32. Cardiac tamponade is difficult to diagnose without echocardiography as many of the features on clinical examination are difficult or impossible to elicit during cardiac arrest.
Tamponde should be considered after penetrating chest trauma or after cardiac surgery.
Treatment is with either needle pericardiocentesis or resuscitative thoracotomy.
33. Drug toxicity is relatively rare unless there is evidence of deliberate overdose.
For in-patients, a review of the patient’s drug chart may be helpful.
34. The next common reversible cause of cardiac arrest is thrombosis. There is no evidence to support the routine thrombolysis of a suspected acute myocardial infarction. If PE is suspected then fibrinolytic therapy can be considered.
Following fibrinolysis during CPR for acute pulmonary embolism, survival and good neurological outcome have been reported in cases requiring in excess of 60 min of CPR. If a fibrinolytic drug is given in these circumstances, consider performing CPR for at least 60–90 min before termination of resuscitation attempts.
35. In the presence of pulseless electrical activity, in skilled hands, ultrasound can be useful for the detection of potentially reversible causes of cardiac arrest (e.g. cardiac tamponade, pulmonary embolism, ischaemia (regional wall motion abnormality), aortic dissection, hypovolaemia, pneumothorax). The integration of ultrasound into advanced life support requires considerable training if interruptions to chest compressions are to be minimised. A sub-xiphoid probe position is recommended. Placement of the probe just before chest compressions are paused for a planned rhythm assessment enables a well-trained operator to obtain views within 10 seconds. The Focused Echocardiography Extended Life Support Course (FEEL-UK) provides a valuable introduction to echocardiography in this setting.
36. A successful resuscitation attempt is one which allows the patient to go home from hospital with no neurological deficit or other functional impairment. Far from being the end of a resuscitation attempt, the return of spontaneous circulation marks the start of the post resuscitation care phase. Careful assessment using the ABCDE approach and application of a post resuscitation care bundle which includes controlled oxygenation and ventilation, identification and treatment of precipitating cause, and consideration of therapeutic hypothermia. Further details of this phase of care are provided in the post resuscitation care lecture.
37. Resuscitation is a team effort. There are several key ingredients that are critical to ensuring safe and effective teamwork.
Pause for a moment to think back to the last cardiac arrest you attended. Give specific consideration to how the resuscitation team functioned. Which things worked well and which things worked less well.
This lecture has so far focused on the technical skills required to resuscitate a patient in cardiac arrest. It is becoming increasingly recognised that the non-technical skills make an important contribution to the overall quality of the resuscitation attempt.
Ideally the team should meet each day, for example, during handover. This will allow for roles to be planned in advance and tasks appropriately allocated.
It is vitally important that a team leader is clearly identified early in the resuscitation attempt. Ideally, as already alluded to, this role should be assigned at the start of the shift.
Specific non-technical skills to consider are:
- task management – identifying and prioritising the necessary tasks
- giving specific tasks to named individuals
- confirming understanding
An example of this is, “George, at the end of the next cycle please give 1 mg adrenaline” as opposed to shouting “1 mg adrenaline” to the team as a whole. Team working involves understanding the strengths and limitations of the team and providing leadership to bring the best out of them. Situational awareness is about being aware of your environment and the interplay between the environment and the team. Decision making is about the cognitive tasks of determining and prioritising relevant treatments. You will learn more about this on the face to face course. I however recommend you review the material in Chapter 2 of the ALS manual and think how these elements interplay with the effective functioning of the resuscitation team.
38. This brings me to the end of this lecture.
The key messages to take away from this lecture are:
- the central role of the ALS algorithm and its role in providing structure and uniformity to a resuscitation attempt
- the importance of delivering of high quality chest compressions with minimal interruptions and avoidance of hyperventilation
- treatment , depending on the underlying rhythm which can be categorised as shockable or non-shockable
- drug treatments in cardiac arrest which are of less importance than good quality CPR and prompt defibrillation
- consideration of the 4 Hs and 4 Ts when thinking about reversible causes of cardiac arrest and, if present, treating them early
- finally, consider the role of non-technical skills in the resuscitation attempt, in particular, effective team leadership and team working.
Credits
Mr Robin Davies is a member of the Resuscitation Council (UK) ALS Subcommittee and BLS/ AED Subcommittee. He contributed to writing the 2010 Guidelines for the International Liaison Committee on Resuscitation (ILCOR). He is the Lead Resuscitation Officer for the ALS e-learning project. He is a Senior Resuscitation Officer at the Heart of England NHS Foundation Trust. (2011).
You have reached the end of this presentation. Either use the controls to revisit the presentation, select Menu to return to the module menu or Home/Exit to return to main course menu.
References
Essentials: Reversible causes
Algorithm: Adult Advanced Life Support Algorithm