- Case study 2

The doctor in charge of the patient’s care carries the legal responsibility for a DNAR decision.
The decisions for a DNAR order can be made on the grounds of:
- Futility (negligible chance of success), or
- The treatment not being in the patient’s best interest, or
- A response to a request from the patient or their legally appointed guardian that they do not wish to be resuscitated
The decision should not be made in isolation and should be clearly documented in the patient’s medical notes. The DNAR order should be regularly reviewed, especially if there is any change in the patient’s condition.
Nurses involved in the patient’s care should be consulted when making a DNAR decisions.
Nurses often provide valuable insight into what is in the patient’s best interest.
Patients’ relatives should be involved whenever possible if a DNAR order is being considered. If the patient is unable to make decisions due to mental incapacity, the Mental Capacity Act requires clinicians to involve relatives or people close to the patient in treatment limitation decisions.
The patient may also have appointed someone to be a personal legal representative in the event of mental incapacity. This representative must be registered with the authorities and always act in the patient’s best interest.
If a doctor considers treatment to be futile, relatives cannot force treatment. However conflict with relatives should be avoided wherever possible. A sensitive discussion about what the process of resuscitation involves will often alleviate concerns, as will assurance that all other relevant treatment and care will continue.
The patient with mental capacity should be central to the DNAR decision making process.
The resuscitation process, risks and benefits should be explained to the patient and their view sought. The exception is where the doctor considers that to offer resuscitation is futile. In this situation, the doctor should sensitively explain the reasons for the decision.
Problems relating to resuscitation decisions most commonly arise from a failure of healthcare staff to communicate effectively with the patient and relatives.
References
- See chapter 16 of the ALS manual for further reading about decisions relating to resuscitation
- Joint statement about decisions relating to cardiopulmonary resuscitation published by the British Medical Association (BMA), the Resuscitation Council (UK) and the Royal College of Nursing (RCN) http://www.resus.org.uk/pages/dnar.htm


- The Resuscitation Council (UK) guidance on the legal status of those who attempt resuscitation http://www.resus.org.uk/pages/legal.htm


- The General Medical Council (GMC) guidance on treatment and care towards the end of life: good practice in decision making www.gmc-uk.org/guidance/ethical_guidance/end_of_life_care.asp


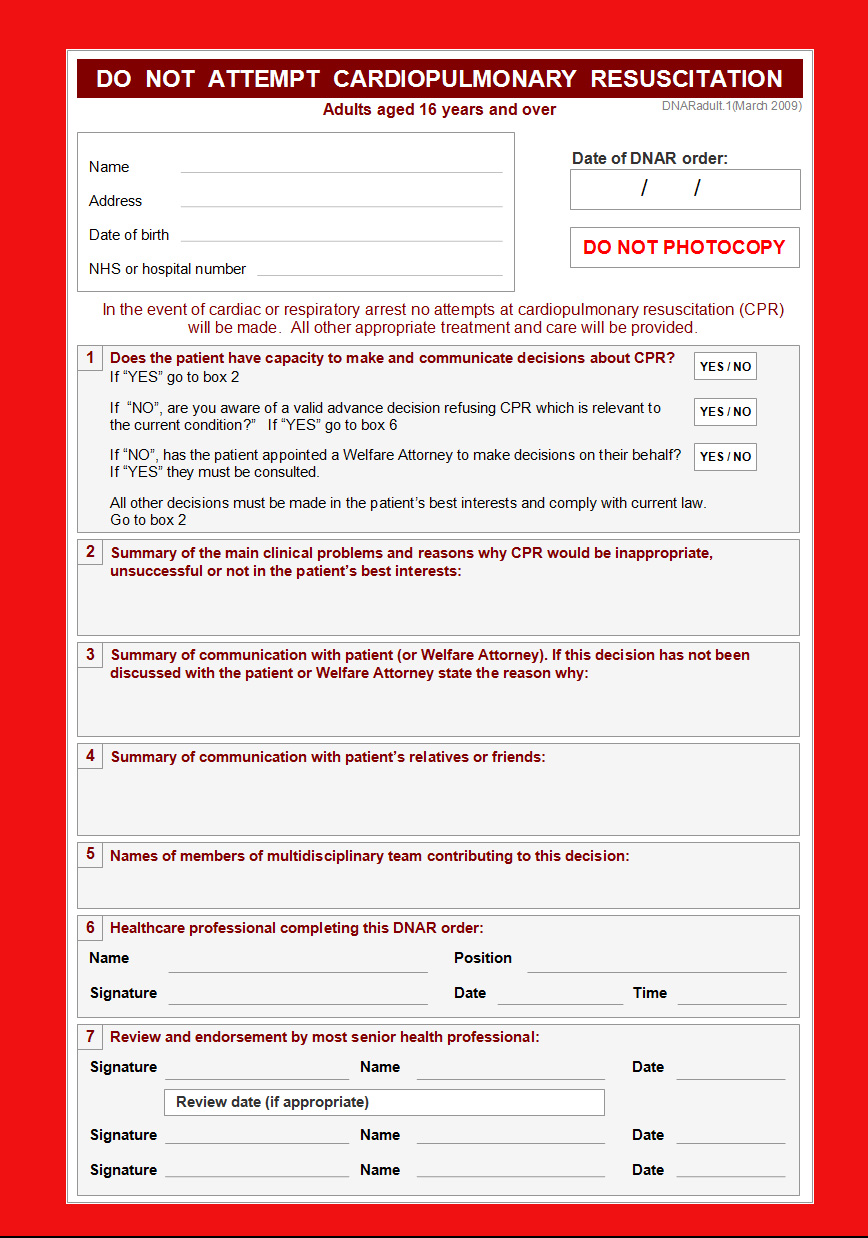
Essentials: Model DNAR forms