- Terminology
Advance decision
The term ‘advance decision’ may apply to any expression of patient preferences. Refusal does not have to be in writing in order to be valid. If patients have expressed clear and consistent refusal verbally, this is likely to have the same status as a written advance decision.
People should ensure that their healthcare team and those close to them are aware of their wishes.
In sudden out-of-hospital cardiac arrest, those attending usually do not know the patient’s situation and wishes and, even if an advance decision has been recorded, it may not be available. In these circumstances CPR can be started immediately and any further information obtained when possible. There is no ethical difficulty in stopping a resuscitation attempt that has started if the healthcare professionals are presented later with a valid advance decision refusing the treatment that has been started.
Advance Decision to Refuse Treatment
Advance Decision to Refuse Treatment
With people who wish to refuse treatment that is potentially life-sustaining, for example ventilation, special rules apply. Their advance decision must be in writing, signed and witnessed.
This document will outline in which specific circumstances the person does not want potentially life sustaining treatment. It can be legally binding if all the specific circumstances that have been identified have been met.
Resuscitation must not be attempted if CPR is contrary to the recorded, sustained wishes of an adult who had capacity and was aware of the implications at the time of making that advance decision.
DNAR and DNACPR
Do not attempt resuscitation and
Do not attempt cardiopulmonary resuscitation
Unfortunately some healthcare providers have mistakenly and inappropriately interpreted the recording of DNAR decisions as indicating that other treatment can or should be withheld. To discourage this it has been suggested that the term DNACPR should be used, to try to emphasise that the recorded decision refers only to the use of CPR and not to any other aspect of treatment that the patient may need.
Do not attempt resuscitation (DNAR) means that in the event of cardiac or respiratory arrest, CPR should not be started - nothing more than that. Other treatment should be continued, including pain relief and sedation, as required. Treatment such as ventilation and oxygen therapy, nutrition, antibiotics, fluid and vasopressors is also continued as indicated. If not, orders not to continue or initiate any such treatments should be made independently of DNAR orders.
Futility
Futility may be considered to exist if resuscitation will not prolong life of a quality that would be acceptable to the patient. Medical futility is the main reason for a DNAR decision.
The overall responsibility for a DNAR decision rests with the senior healthcare professional in charge of the patient, after appropriate consultation with other healthcare professionals involved in the patient’s care. This type of decision is often complex and should be undertaken by senior, experienced members of the medical team.
References
- See chapter 16 of the ALS manual for further reading about decisions relating to resuscitation
- Joint statement about decisions relating to cardiopulmonary resuscitation published by the British Medical Association (BMA), the Resuscitation Council (UK) and the Royal College of Nursing (RCN) http://www.resus.org.uk/pages/dnar.htm


- The Resuscitation Council (UK) guidance on the legal status of those who attempt resuscitation http://www.resus.org.uk/pages/legal.htm


- The General Medical Council (GMC) guidance on treatment and care towards the end of life: good practice in decision making www.gmc-uk.org/guidance/ethical_guidance/end_of_life_care.asp


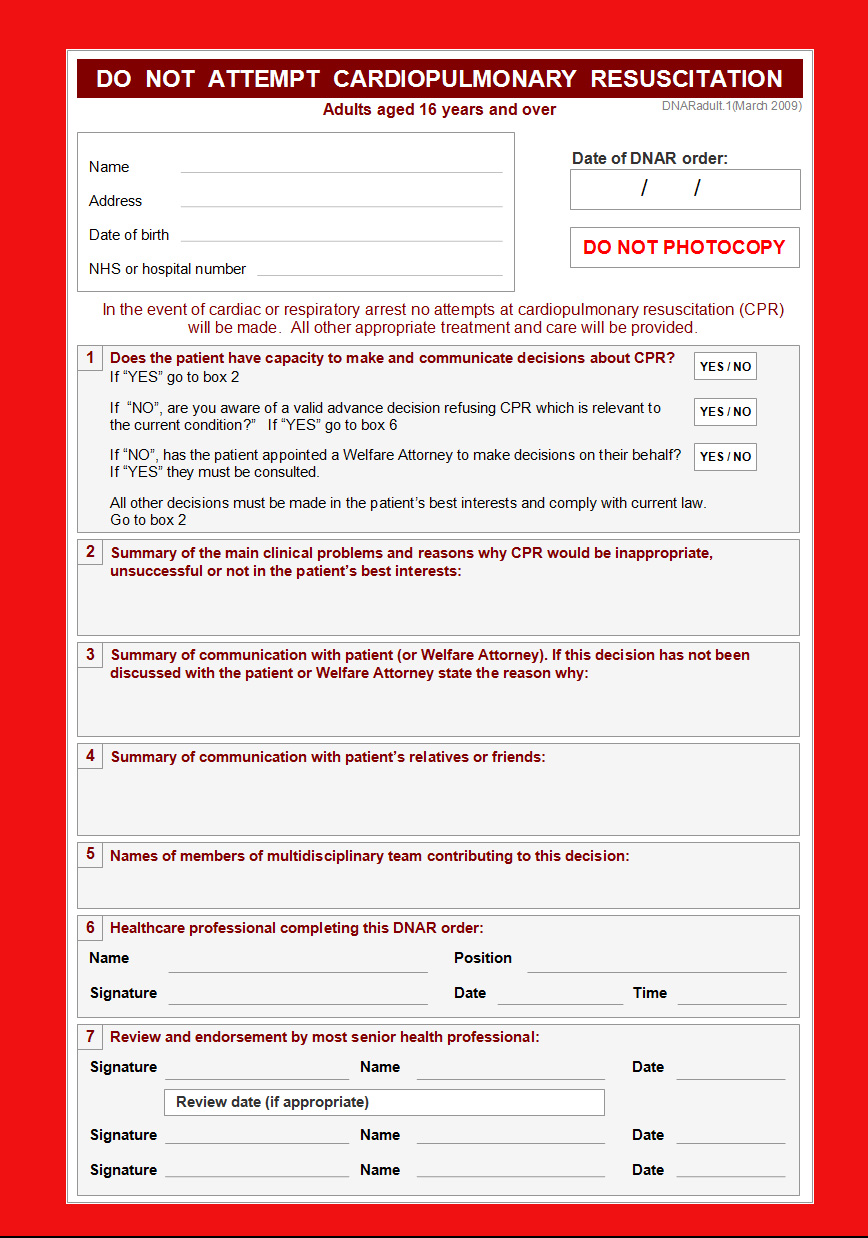
Essentials: Model DNAR forms