
- The 5-step approach
The most efficient way to interpret ABG analysis is by strictly following five simple steps.
Step one – how is the patient?
This will often provide clues to help with interpretation of the results. For example after a cardiac arrest, a metabolic acidosis might be expected as a result of anaerobic respiration during the arrest producing lactic acid. A patient with a well-compensated chronic condition will usually display clues about the primary cause and secondary compensation.
This will often provide clues to help with interpretation of the results. For example after a cardiac arrest, a metabolic acidosis might be expected as a result of anaerobic respiration during the arrest producing lactic acid. A patient with a well-compensated chronic condition will usually display clues about the primary cause and secondary compensation.

Step two – is the patient hypoxaemic?
A patient’s PaO2 should normally be between 10.0-13.0 kPa when breathing air. However, if the patient is receiving supplemental oxygen the PaO[sub]2[/sub] must be interpreted in light of the inspired oxygen concentration.
If there is a numerical difference of greater than 10 between the inspired concentration (%) and the arterial partial pressure of oxygen, then there is a defect in oxygenation proportional to the magnitude of the difference.
A patient’s PaO2 should normally be between 10.0-13.0 kPa when breathing air. However, if the patient is receiving supplemental oxygen the PaO[sub]2[/sub] must be interpreted in light of the inspired oxygen concentration.
If there is a numerical difference of greater than 10 between the inspired concentration (%) and the arterial partial pressure of oxygen, then there is a defect in oxygenation proportional to the magnitude of the difference.
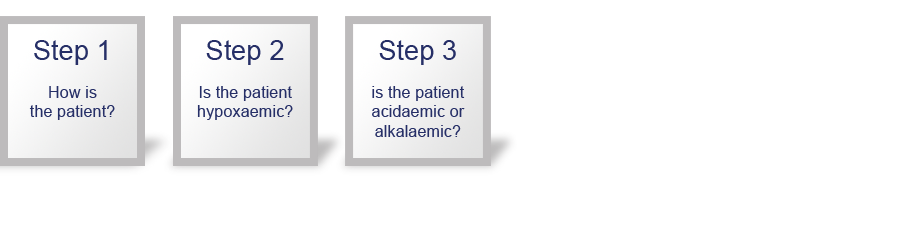
Step three – is the patient acidaemic (pH <7.35) or alkalaemic (pH> 7.45)?
If the pH is within or very close to the normal range then this suggests normality or a chronic condition with full compensation. In principle, the body never overcompensates and this should enable the primary problem to be determined.
If the pH is within or very close to the normal range then this suggests normality or a chronic condition with full compensation. In principle, the body never overcompensates and this should enable the primary problem to be determined.
![A flow diagram that represents the 5-step approach. The following boxes are currently on screen: Step one – how is the patient?, Step two – is the patient hypoxaemic?, Step three – is the patient acidaemic (pH <7.35) or alkalaemic (pH> 7.45)?, Step four – what happened to the PaCO[SUB]2[/SUB]?<br/> A flow diagram that represents the 5-step approach. The following boxes are currently on screen: Step one – how is the patient?, Step two – is the patient hypoxaemic?, Step three – is the patient acidaemic (pH <7.35) or alkalaemic (pH> 7.45)?, Step four – what happened to the PaCO[SUB]2[/SUB]?<br/>](images/m35_t05_010_4.png)
Step four – what has happened to the PaCO2?
Is the abnormality wholly or partially due to a defect in the respiratory system?
If the pH is <7.35 ( acidaemia):
Is the PaCO[sub]2[/sub] increased (>6.0 kPa)?
If so, there is a respiratory acidosis that may be accounting for all or part of the derangement. There could also be a metabolic component (see step 5).
If the pH is > 7.45 (alkalaemia):
Is the PaCO[sub]2[/sub] reduced (<4.7 kPa)?
If so, there is a respiratory alkalosis. This is an unusual finding in a patient breathing spontaneously with a normal respiratory rate.
Is the abnormality wholly or partially due to a defect in the respiratory system?
If the pH is <7.35 ( acidaemia):
Is the PaCO[sub]2[/sub] increased (>6.0 kPa)?
If so, there is a respiratory acidosis that may be accounting for all or part of the derangement. There could also be a metabolic component (see step 5).
If the pH is > 7.45 (alkalaemia):
Is the PaCO[sub]2[/sub] reduced (<4.7 kPa)?
If so, there is a respiratory alkalosis. This is an unusual finding in a patient breathing spontaneously with a normal respiratory rate.
![<p>A flow diagram that represents the 5-step approach. The following boxes are currently on screen: Step one – how is the patient?, Step two – is the patient hypoxaemic?, Step three – is the patient acidaemic (pH <7.35) or alkalaemic (pH> 7.45)?, Step four – what happened to the PaCO[sub]2[/sub]? and Step five – what has happened to the base excess (BE)<i> </i>or bicarbonate?<b></b></p><p></p> <p>A flow diagram that represents the 5-step approach. The following boxes are currently on screen: Step one – how is the patient?, Step two – is the patient hypoxaemic?, Step three – is the patient acidaemic (pH <7.35) or alkalaemic (pH> 7.45)?, Step four – what happened to the PaCO[sub]2[/sub]? and Step five – what has happened to the base excess (BE)<i> </i>or bicarbonate?<b></b></p><p></p>](images/m35_t05_010_5.png)
Step five – what has happened to the base excess (BE) or bicarbonate?
Is the abnormality wholly or partially due to a defect in the metabolic system?
If the pH is <7.35 ( acidaemia):
Is the base excess (BE) reduced (more negative than -2 mmol l-[sup]1[/sup]) and/or the bicarbonate reduced (<22 mmol l[sup]-[/sup][sup]1[/sup])?
If so, there is a metabolic acidosis accounting for all or part of the derangement.
If the pH is > 7.45 (alkalaemia):
Is the base excess (BE) increased (> +2 mmol l[sup]-[/sup][sup]1[/sup]) and/or the bicarbonate increased (>26 mmol l[sup]-[/sup][sup]1[/sup])?
If so, there is a metabolic alkalosis accounting for all or part of the derangement.
Is the abnormality wholly or partially due to a defect in the metabolic system?
If the pH is <7.35 ( acidaemia):
Is the base excess (BE) reduced (more negative than -2 mmol l-[sup]1[/sup]) and/or the bicarbonate reduced (<22 mmol l[sup]-[/sup][sup]1[/sup])?
If so, there is a metabolic acidosis accounting for all or part of the derangement.
If the pH is > 7.45 (alkalaemia):
Is the base excess (BE) increased (> +2 mmol l[sup]-[/sup][sup]1[/sup]) and/or the bicarbonate increased (>26 mmol l[sup]-[/sup][sup]1[/sup])?
If so, there is a metabolic alkalosis accounting for all or part of the derangement.
Select Next to continue.
References
See chapter 15 of the ALS manual for further reading about arterial blood gas analysis.
Essentials: 5-step approach to ABG interpretation
Step 1 – how is the patient?
Step 2 – is the patient hypoxaemic?
Step 3 – is the patient acidaemic or alkalaemic?
Step 4 – what happened to the PaCO2?
Step 5 – what has happened to the base excess (BE) or bicarbonate?
Settings
Font colour
default inverted high contrast high contrast inverted high contrast soft green on blackSample text
text looks like thisTEXT LOOKS LIKE THIS
